14-year review of cancer screening rates: How have breast, prostate, cervical and colorectal cancer screening rates risen by 2024

The COVID-19 pandemic disrupted routine cancer screenings. How do screening rates compare before and after the pandemic? We examined data from 2011 to 2024 on breast, cervical, prostate, and colorectal cancer screenings, uncovering key insights into which rates returned to or exceeded pre-pandemic levels by 2024, and which did not.
Authors
Discovery Health Intelligence Team members: Sian-Ailin Da Silva (Statistician), Claudia Pastellides (Actuary), Lizelle Steenkamp (Senior Healthcare Statistician) and Lara Wayburne (Chief Health Intelligence Actuary)
Quick Overview
Cancer is one of the most prevalent and high-costing conditions claimed for by Discovery Health Medical Scheme (DHMS) members. The Scheme offers a range of cancer screening benefits to encourage members to adhere to routine checks that either prevent cancer (such as for cervical cancer) or allow for the earliest possible detection of cancer. We analysed cancer screening rates from 2011 to 2024 for breast, cervical, prostate and colorectal cancers.
Overall, the recovery in screening rates post-pandemic for most cancers is a positive sign, highlighting the resilience of healthcare systems and the importance of routine cancer screenings in early detection and prevention. Continued efforts are necessary to increase cervical cancer screening and ensure that members utilize these critical preventive services.
Breast cancer screening rates, measured by mammograms claimed for, have been increasing steadily, with a 1.0% annual increase from 2011 to 2016. Screening rates had recovered to pre-pandemic levels by 2024 (also factoring in the effects a Scheme benefit change for mammography in 2017). From 2019 (pre-pandemic) to 2024, prostate cancer screening rates showed a robust recovery at 8.9% higher than pre-pandemic levels, and colorectal cancer screening rates were up 26.3%. However, cervical cancer screening rates hadn't recovered to pre-pandemic levels, remaining at 9.1% lower than they were in 2019.
From 2011 to 2024 cancer prevalence has increased by 7.6% per annum for Discovery Health Medical Scheme members
The Discovery Health Medical Scheme (DHMS) is one of the Schemes administered by Discovery Health. Between 1 October 2023 and 30 September 2024 records show 64,573 Scheme members claimed for cancer-related services.
Looking at the same rolling period over the years 2011 to 2024, the number of medical scheme members who have cancer (cancer prevalence) has grown by 7.6% per annum, with an associated 12.1% per annum cost increase for their direct oncology treatment costs. Cancer is one of the most prevalent and high-costing conditions claimed for by members.
It's globally evident that, throughout the pandemic period, routine preventive health checks across a range of conditions were postponed or cancelled - including for cancer. Understandably, people feared exposure to COVID-19 at healthcare facilities, alongside the need to prioritise COVID-19 care overall. Analysis of DHMS member data shows this trend too, as cancer screening rates declined during the COVID-19 period.
- DHMS offers a range of cancer screening benefits to encourage members to perform routine checks that either prevent cancer (such as for cervical cancer) or allow for the earliest possible detection of cancer. For those diagnosed with cancer, there is access to a comprehensive basket of care through the DHMS Oncology Programme.
What did we set out to investigate?
We set out to investigate cancer screening rate trends over time, using the rolling period mentioned above - 1 October 2011 to 30 September 2024 (also with a focus on 2019 to 2020 which was the year the COVID-19 pandemic started).
We included the following cancers in our analysis (as these are some of the most prevalent cancers among DHMS members):
- Breast cancer
- Cervical cancer
- Prostate cancer
- Colorectal cancer
Cancer screening trends among Discovery Health Medical Scheme members over time
1. Breast cancer screening trends
Breast cancer is the most common primary cancer for female DHMS members. Approximately 2,263 DHMS members were diagnosed with breast cancer between 1 October 2023 and 30 September 2024.
World Health Organisation (WHO) guidelines advise that women aged 40 years or older have breast cancer screening (mammography) once every two years. DHMS benefits align with the frequency of 2 years for members who are not considered to be high risk.
We use claims for mammograms to show screening for breast cancer.
For our study period - 2011 to 2024 - and for the rolling 12 months from the start of October to the end of September for each year, we counted the number of eligible members (females over 40 years of age) who'd had a mammogram in the recommended time (i.e. past 26 months - allowing for 2 months leeway considering members may not always screen exactly 2 years post their last mammogram). Members who had not been with DHMS for at least 2 years were excluded from the analysis.
- The above-mentioned methodology was applied to our analysis of every screening check considered for this report.
Before 2017 the DHMS Screening and Prevention benefit funded annual mammograms for eligible women. In 2017, in line with WHO recommendations, mammogram funding was adjusted to provide screening every two years for members with average breast cancer risk, and once a year for high-risk members.
- In 2017, the MyFamilyHistory tool, a risk-assessment questionnaire, was also released as a means through which to assess DHMS members' risk.
Figure 1 shows that mammography rates per 1,000 eligible person years have been increasing steadily.
- 'Rates per 1,000 person years' means we count the number of screening episodes per 1,000 years of combined time over which people included in the study are being looked at - for example, 1,000 people observed for 1 year is 1,000 person years.
There was a 1.0% increase per year from 2011 to 2016. With the 2017 change in the DHMS mammography benefit referred to above, we marked a decline in mammography screening rates between 2016 and 2019, from 310.3 to 292.2 screening checks per 1,000 eligible person years.
From 2019 to 2020 (the first year of COVID-19) screening rates decreased by 7.3% - from 292.2 down to 270.8 per 1,000 eligible person years. Rates dropped by a further 6.1% in 2021 to 254.4 per 1,000 eligible person years (a drop of 13.4% across both years).
Then, there was a slight increase in screening rates from 2021 to 2022, and by 2024 screening rates had recovered to levels higher than they were in 2019 (pre-pandemic).
In fact, in 2024, screening rates exceeded 2019 rates by 6.1% at 310.0 screens per 1,000 eligible person years.
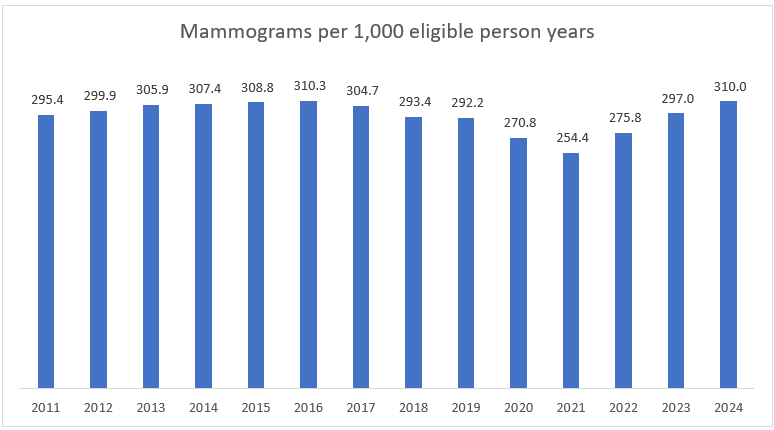
Figure 1: Breast cancer screening rates per 1,000 eligible person years (females aged 40 years or older)
2. Cervical cancer screening trends
We recorded 109 DHMS members diagnosed with cervical cancer between 1 October 2023 and 30 September 2024.
WHO guidelines advise that women aged 30 and older should undergo cervical cancer screening either by having
- A pap smear every 3 to 5 years or;
- HPV screening test (newer, preferred method) done every 5 to 10 years.
DHMS members have access to cover for a pap smear once every three years or an HPV test once every five years.
For each month over our study period, we counted the number of eligible members (females over 30 years of age) who'd had a pap smear or HPV test in the recommended time (i.e. past 38 months - allowing two months leeway considering members may not always screen exactly three years later). Any member who hadn't been with the Scheme for at least three years was excluded.
Among DHMS scheme members, cervical cancer screening rates have typically been higher than mammography rates over the study period (see Figure 2) - meaning more women have this kind of screening check.
However, focusing on cervical cancer screening rates shows a slow and steady decline from 2011 to 2019, and a marked decline in the years affected by the COVID-19 pandemic (2020 - 2022).
During the pandemic years, cervical cancer screening rates decreased by 5.0% from 2019 to 2020, by a further 3.9% from 2020 to 2021 and by 2.6% more in 2022 (from 410.5 per 1,000 eligible person years in 2019 to 365.2 per 1,000 eligible person years in 2022). There was a slight recovery in screening rates from 2022 to 2023 (1.8%) and a further recovery of 0.4% in 2024 (to 373.2 per 1,000 eligible person years).
Unlike mammography rates, cervical cancer screening rates had, by 2024, not recovered from the decrease experienced through the pandemic period, remaining below pre-COVID-19 levels (9.1% lower than 2019 screening rates).
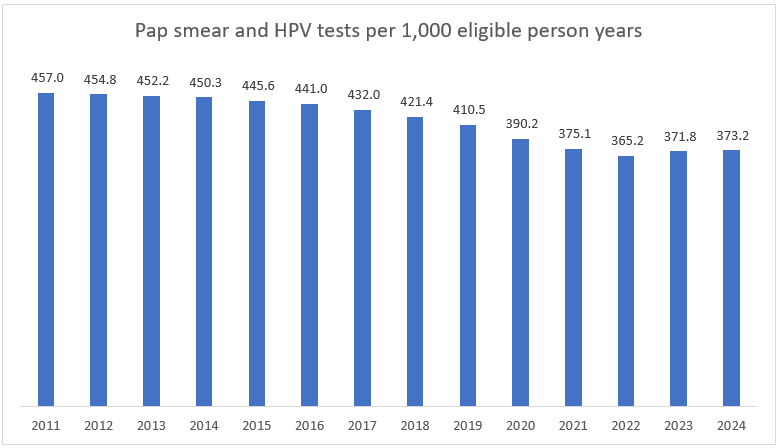
Figure 2: Cervical cancer screening rates per 1,000 eligible person years (females aged 30 years or older)
3. Prostate cancer screening trends
Prostate cancer is the most common primary cancer among male DHMS members.
We recorded 2,458 DHMS members diagnosed with prostate cancer between 1 October 2023 and 30 September 2024. For the first time in DHMS history, new prostate cancer diagnoses exceeded new breast cancer diagnoses - a trend maybe driven by an ageing member base and increasing screening rates.
Male DHMS members have cover for annual prostate cancer screening. We have classified claims for prostate specific antigen (PSA) testing as related to screening for prostate cancer (for members that are not yet enrolled on the oncology benefit).
The USPSTF (US Preventative Services Task Force) recommends prostate screening for men aged from 55 to 69 years in discussion with their treating clinicians after weighing the benefits versus the risks of screening.
Figure 3 shows that between 2011 and 2019, prostate cancer screening rates increased year-on-year - with an annualised increase of 1.5% per annum.
In 2020, the first year of the pandemic, prostate screening rates fell by 8.2% compared to 2019 rates - from 465.4 to 427.1 screens per 1,000 eligible people years but almost recovered by the end of September 2021 to 456.2 screens per 1,000 eligible person years. Rates increased to above pre-pandemic levels in 2022. And by the end of September 2024, screening rates were at 506.8 screens per 1,000 eligible person years in 2024 - 8.9% higher than pre-pandemic levels.
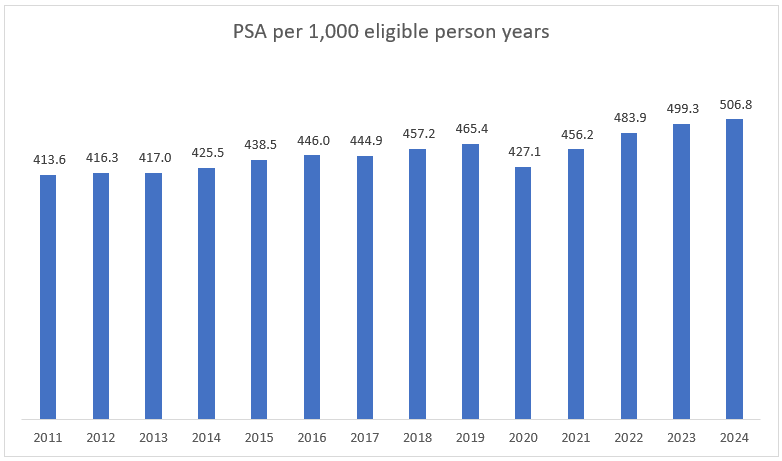
Figure 3: Prostate cancer screening rates per 1 000 eligible person years (males aged 55 - 69)
4. Colorectal cancer screening trends
After breast cancer and prostate cancer, colorectal cancer is the third most prevalent cancer among DHMS members. There were approximately 1027 new colorectal cancer registrations between 1 October 2023 and 30 September 2024.
People aged 50 years or older are eligible for colorectal cancer screening every 2 years. The colorectal screening benefit was introduced in 2019. DHMS members from 45 to 75 years old have access to cover for bowel cancer screening every two years.
We have classified claims for faecal occult blood (chemical or monoclonal antibody) tests as screening for colorectal cancer.
Figure 4 shows that colorectal cancer screening showed a steady increase year-on-year from 2011 to 2019. Then, from 2019 to 2020, screening rates dropped slightly by 2% - from 25.5 to 24.9 per 1,000 eligible person years. In 2021, screening rates quickly recovered back to pre-pandemic levels (27.3 screens per 1,000 eligible person years) and were 26.3% higher by the end of September 2024 than for 2019 at 32.3 screens per 1,000 eligible person years.
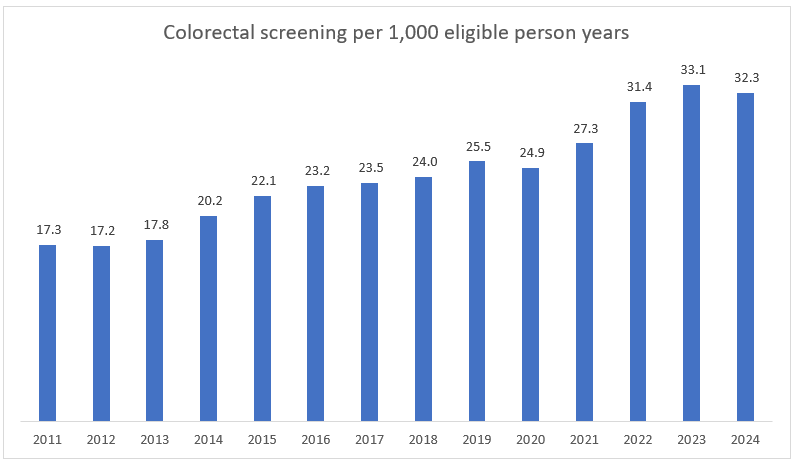
Figure 4: Colorectal screening rates per 1,000 eligible person years (aged 50 years or older)
Conclusion
The COVID-19 pandemic significantly disrupted routine cancer screenings, leading to notable declines in screening rates for breast, cervical, prostate, and colorectal cancers among eligible DHMS members, as for people across the world. However, our analysis shows a promising recovery in screening rates by 2024, for most cancer types.
Breast cancer screening rates, which had declined during the pandemic, have not only recovered but surpassed pre-pandemic levels by 2024, reaching 310.0 screens per 1,000 eligible person years - in fact nearing 2016 levels at 6.1% higher than pre-pandemic levels.
Prostate cancer screening rates also showed a robust recovery, with rates increasing to 506.8 screens per 1,000 eligible person years in 2024, 8.9% higher than pre-pandemic levels.
Colorectal cancer screening rates followed a similar trend, with a 26.3% increase compared to 2019, reaching 32.3 screens per 1,000 eligible person years by the end of September 2024.
In contrast, cervical cancer screening rates had by 2024 not fully recovered to pre-pandemic levels. Despite a slight recovery from 2022 to 2024, rates remained 9.1% lower than in 2019, at 373.2 screens per 1,000 eligible person years. Efforts to target interventions that encourage cervical cancer screening among DHMS members remains important. Further investigation is needed to better understand these trends.
Overall, the recovery in screening rates for most cancers is a positive sign, highlighting the resilience of healthcare systems and the importance of routine cancer screenings in early detection and prevention. Continued efforts are necessary to address the gaps in cervical cancer screening and ensure that all members utilise these critical preventive services.
Interested in knowing more or reporting on these findings?
Please contact us on MEDIA_RELATIONS_TEAM@discovery.co.za to request any updated data available since publication and to obtain any further context required.
Did you find this post interesting?
Please visit our Discovery Health Insights Hub for a range of analyses and insights shared by our Discovery Health Intelligence Team over the past three and a half years and spanning a variety of health-related themes.
All information shared on this page is based on perspectives gained from analysing data acquired by Discovery Ltd and its various affiliate entities (Discovery). The analysis, which is conducted by Discovery's actuarial and data science team, aims to encourage industry dialogue. Publications containing our analyses are shared for educational and informational purposes only. Each publication reflects only the data available for analysis at the time of publication. It does not, unless otherwise indicated, constitute peer-reviewed, published scientific research, and hence should not be interpreted as such or used as a basis for altering treatment decisions. While every effort has been made to ensure the accuracy of the content conveyed, we cannot be held liable or responsible for any actions or decisions taken based on the information shared in this article.